- Home
- Foot & Ankle Conditions
- Arch Conditions: Flat Feet and Cavus Foot
Arch Conditions: Flat Feet and Cavus Foot
Flat foot vs. cavus foot
Flatfoot and cavus foot describe several complex foot disorders, each with its own causes and symptoms.
If you have flat feet, also known as pes planus, you will have a very low arch or no arch at all, meaning one or both of the soles of your feet press flat on the ground.
Cavus foot is the exact opposite of flat foot and occurs when the arch is higher than normal. It's also known as pes cavus and much like flat foot, it can cause a number of issues, including pain in the foot, hips, knees, and lower back.
- What are flat feet?
- What are the symptoms of flat feet?
- How is flatfeet diagnosed?
- How is flatfoot treated?
- What is a cavus foot?
- What are the symptoms of cavus foot?
- What are common causes of cavus foot?
- What are the treatment options for cavus foot?
- Why UFAI is the best choice for your foot care
- Flat feet and cavus feet FAQs
- What are the best shoes for flat feet?
- Are flat feet genetic?
- Can flat feet cause knee pain?
- Can flat feet cause back pain?
- Can flat feet cause shin splints?
- Can flat feet cause plantar fasciitis?
- What are the best shoes for high arches?
-
Foot and Ankle Surgeon and Co-Director of University Foot and Ankle Institute
Board-Certified Podiatric Foot and Ankle Specialist, Dr. Gary Briskin, DPM, FACFAS, began his medical training by serving a residency at Flint General Hospital in Michigan. Once completed, he established a practice in Century City Hospital, where he soon became chief of podiatric surgery.
Dr. Briskin is a Diplomat of the American Board of Podiatric Surgery and a Fellow of the American College of Foot and Ankle Surgeons. He also serves as an assistant clinical professor at the UCLA School of Medicine and is co-founder and co-director of University Foot and Ankle Institute.
 I been going to University Foot and Ankle Institute for a few years now. I picked this foot doctor due to the excellent review...Larry B.
I been going to University Foot and Ankle Institute for a few years now. I picked this foot doctor due to the excellent review...Larry B. Great experience. Great communication. Great direction for my care. Very happy I chose to go with this particular doctor and o...Christopher R.
Great experience. Great communication. Great direction for my care. Very happy I chose to go with this particular doctor and o...Christopher R. Great service and care. Highly recommend Dr. Franson.David B.
Great service and care. Highly recommend Dr. Franson.David B. I wish I could give Dr. Justin Franson 10 stars. I went with him because a friend recommended it to me.I broke my ankle back in...Fabiana P.
I wish I could give Dr. Justin Franson 10 stars. I went with him because a friend recommended it to me.I broke my ankle back in...Fabiana P. If you have to go see a Doctor than this is a great experience.Frank M.
If you have to go see a Doctor than this is a great experience.Frank M. My doctor was great. Really greatRudolph B.
My doctor was great. Really greatRudolph B. Excellent place to get your feet looked at and evaluated!
Excellent place to get your feet looked at and evaluated!
I highly recommend this office!!!
Excellent Doctors and assistants!
T...Hope L. Good.David E.
Good.David E. Your Santa Barbara office and Dr. Johnson always give me excellent care!Jayne A.
Your Santa Barbara office and Dr. Johnson always give me excellent care!Jayne A. Dr. Gina Nalbadian was amazing!! I came in with an emergency foot situation and she had wonderful bedside manner and resolved m...Danielle C.
Dr. Gina Nalbadian was amazing!! I came in with an emergency foot situation and she had wonderful bedside manner and resolved m...Danielle C. I was frustrated that after 3 weeks I still hadn’t heard back about my PT referral status. And I did sit in a room for over 30 ...Sarah C.
I was frustrated that after 3 weeks I still hadn’t heard back about my PT referral status. And I did sit in a room for over 30 ...Sarah C. I’m very pleased with Dr. Kelman.Alan S.
I’m very pleased with Dr. Kelman.Alan S.
-
 Listen Now
Custom Orthotics vs. Over-the-Counter Inserts: Which Are Best for Your Feet?
Read More
Listen Now
Custom Orthotics vs. Over-the-Counter Inserts: Which Are Best for Your Feet?
Read More
-
 Listen Now
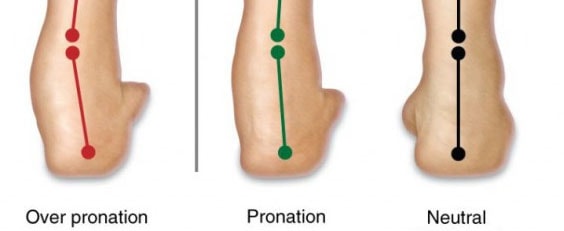
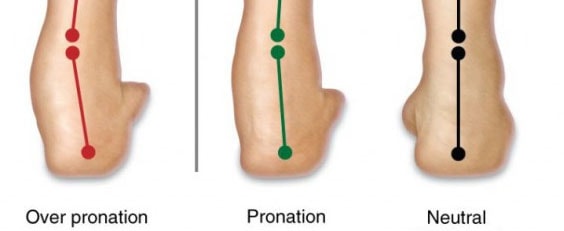
Overpronation: What Is It and How Can You Correct It?
Read More
Listen Now
Overpronation: What Is It and How Can You Correct It?
Read More
-
 Listen Now
How Carrying Extra Weight Affects Your Feet and Ankles
Read More
Listen Now
How Carrying Extra Weight Affects Your Feet and Ankles
Read More
-
![Flatfoot Reconstruction Is Best Option For Patients Of Any Age [New Study]](//ufai.cachefly.net/blog/wp-content/uploads/2018/04/Flat-Foot-Reconstructive-Surgery.jpg) Listen Now
Flatfoot Reconstruction Is Best Option For Patients Of Any Age [New Study]
Read More
Listen Now
Flatfoot Reconstruction Is Best Option For Patients Of Any Age [New Study]
Read More
-
 Listen Now
The Power of Pediatric Flexible Flatfoot Procedures
Read More
Listen Now
The Power of Pediatric Flexible Flatfoot Procedures
Read More
-
 Listen Now
Worried About Your Wide Feet? Don't Be!
Read More
Listen Now
Worried About Your Wide Feet? Don't Be!
Read More
-
 Listen Now
All About Foot Arch Pain and Foot Arch Cramps
Read More
Listen Now
All About Foot Arch Pain and Foot Arch Cramps
Read More
-
 Listen Now
How to Choose Running Shoes: 6 Essential Steps
Read More
Listen Now
How to Choose Running Shoes: 6 Essential Steps
Read More



![Flatfoot Reconstruction Is Best Option For Patients Of Any Age [New Study]](http://ufai.cachefly.net/blog/wp-content/uploads/2018/04/Flat-Foot-Reconstructive-Surgery.jpg)



