What is cellulitis of the foot?
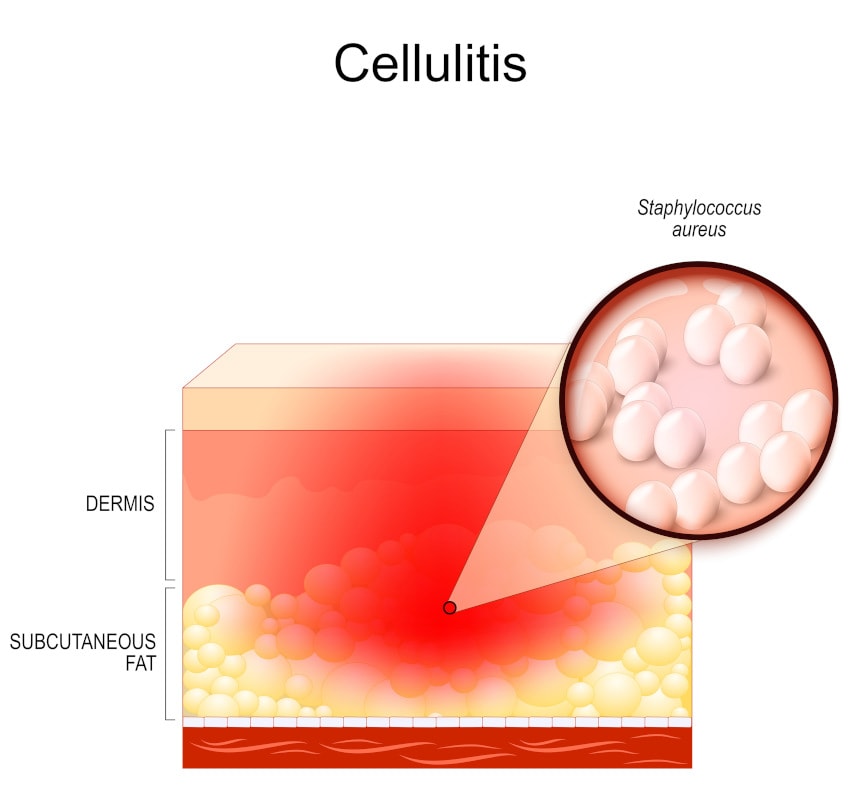
Cellulitis is a common bacterial infection of the skin and soft tissues. In the U.S., we have over 14 million cases of cellulitis each year! While it is usually superficial, it can become severe and life-threatening if left untreated.
Cellulitis can occur on any part of the body, but is most common on the toes, feet, and legs. Often painful, cellulitis first manifests as a discolored area of skin that can spread quickly. The infected area of your foot or lower leg will be hot or tender to the touch. If left untreated, the infection can spread to the lymph nodes or bloodstream, so contact your healthcare provider immediately if you notice any symptoms.
What are the symptoms of cellulitis in the foot?
Cellulitis is a bacterial skin infection, so it shares symptoms with any other infection. Symptoms to watch out for include:
- Pain and tenderness
- Redness or inflammation
- Sores or rashes that grow quickly
- Expanding discoloration and swelling
- Fever
What causes cellulitis in the foot?
The most common types of bacteria that cause cellulitis are Staphylococcus (staph) and Streptococcus (strep). The incidence of methicillin-resistant Staphylococcus aureus (MRSA) — a more serious, antibiotic-resistant staph infection — has been increasing, complicating treatment options. These bacteria enter the body through damaged skin.
Risk factors for cellulitis include:
- dry, cracked skin
- puncture wound
- insect bites and stings
- human or animal bites
- skin conditions such as eczema
- poor circulation
- lymphedema (problems with the lymphatic system)
- chronic edema (swelling) of the lower legs
- medical conditions that weaken the immune system
Can athlete’s foot cause cellulitis?
In short: yes. Athlete’s foot is a fungal infection, not a bacterial one, but it can cause cracks and (rarely) blisters. These breaks in the skin provide an entry point for cellulitis-causing bacteria.
What is diabetic foot cellulitis?
While not a direct cause, diabetes can increase your risk of cellulitis. The weakened immune system from diabetes increases your general risk of infection. To make matters worse, diabetic neuropathy in the feet puts you at an even higher risk of cellulitis.
Cellulitis of the foot in diabetic patients can quickly escalate if not caught early. With diabetic neuropathy, foot injuries can go unnoticed due to a lack of pain sensation. Unnoticed injuries can easily become infected and a weakened diabetic immune system allows that infection to quickly spread.
What are the risks of cellulitis?
Infections are risky business; you should contact a healthcare professional as soon as you notice signs of infection.
If left untreated, cellulitis can spread into the bloodstream and to other parts of your body. Untreated cellulitis can also escalate into sepsis (also known as “blood poisoning”) or endocarditis (inflammation of the heart).
How to prevent cellulitis of the foot
While cellulitis is painful and dangerous, it is also preventable. There is no vaccine against these bacteria, but cellulitis can be prevented through proper wound care. When you injure your foot or leg, follow these precautions:
- Wash the skin injury regularly with warm water and gentle soap.
- Cover the wound with a fresh bandage daily. You may have heard an open wound needs to “air out,” but it’s really the opposite!
- Watch for signs of infection. Check daily for redness, pain, or pus. If you notice signs of infection — call your doctor.

Another way to prevent cellulitis foot infection is to protect your feet. Easy preventative foot care includes:
- Proper skin care. Moisturizing your feet regularly with lotions or ointments prevents cracks and protects against infection.
- Proper footwear. Shoes protect your feet from dirt, rocks, and stubbed toes. Well-fitting shoes prevent chafing and blisters.
- Nail maintenance. Sharp toenails can cut their neighboring toes, creating an entrance for bacteria. Poorly maintained toenails can also become ingrown, increasing your risk of infection.
- Daily monitoring. Patients with diabetes or nerve damage should examine their feet daily for new cuts, scrapes, blisters, or ulcers.
Cellulitis foot treatment options
First, we’ll examine the affected area to rule out other skin conditions such as dermatitis or erysipelas (a less severe form of cellulitis). We may take a swab of the affected skin to determine the exact cause of infection.
The first line of treatment for cellulitis is oral antibiotics. Severe cases may require intravenous antibiotics — or even surgical intervention.
If you have an abscess, we will professionally drain it. Don’t try to drain an abscess yourself, or you may experience reinfection.
Why trust University Foot and Ankle Institute with your foot and ankle health?
The expert DPMs at UFAI are trained in all areas of foot and ankle health. From cellulitis treatment to plantar fasciitis pain, to toenail maintenance and physical therapy, our podiatrists can handle any problem your feet are having.
At UFAI patients always receive personalized ankle and foot care from our internationally recognized foot and ankle professionals. We treat you as an individual, not just another patient. In creating an infection treatment plan, we consider your physical activities, profession, and what you expect to see as the result of our treatment.
For a consultation, call (877) 736-6001 or make an appointment online now.
Our podiatrists take patients’ safety seriously. Our podiatry facility’s Covid-19 patient safety procedures exceed all the CDC’s coronavirus pandemic recommendations. Masks are always required in our institutes.
University Foot and Ankle Institute is conveniently located throughout Southern California and the Los Angeles area as our foot doctors are available at locations in or near Santa Monica, Beverly Hills, West Los Angeles, Manhattan Beach, Northridge, Downtown Los Angeles, Westlake Village, Granada Hills, and Valencia.
- Could Feet Be the Windows to Your Health? - May 24, 2024
- Is Foot Analysis Better than Horoscopes? What Do Your Toes Reveal About Your Personality? - May 7, 2024
- The Link Between Foot Health and Posture - April 14, 2024